What is Insulin Resistance & How is It Managed?
February 26th, 2025 | 13 min. read

Some Ask Monica episodes may contain references to our previous name, RMA of CT. Learn more here.
In this article:
- Insulin Resistance 101
- Symptoms of Insulin Resistance
- Type 2 Diabetes & Insulin Resistance
- Are insulin resistance and prediabetes the same thing?
- The Connection Between Diabetes & Fertility
- What is insulin resistance?
- How Insulin Works
- Understanding Insulin Resistance
- How Insulin Resistance Affects the Body
- How does insulin resistance cause weight gain?
- Ways to Treat Insulin Resistance
Insulin Resistance 101
As a fertility nurse, health coach, and someone who battles insulin resistance daily, I only teach the principles I live by. I understand the big lifestyle shifts many people need to make when trying to prevent diabetes, and it isn’t always easy.
But I’m here for you – helping you make one simple change, little by little, building up a lifestyle that both prevents diabetes and makes you feel good. The key to creating lasting change is first understanding what’s happening.
Let's discuss what insulin resistance is, its connection with fertility, how it impacts your body, and some ways to combat and manage its symptoms.
Symptoms of Insulin Resistance
In some people, insulin resistance may not have any physical symptoms. In others, these common signs of the condition may be noticeable:
- Acanthosis nigricans (dark, velvety patches of skin in body folds and creases)
- Skin tags
- Blurred vision
- Weight gain
- Irregular menstrual periods
What are the risk factors for insulin resistance?
Risk factors for insulin resistance include family history, genetics, your age, lifestyle and diet, physical inactivity, and carrying excess weight.
Does insulin resistance ever go away?
While insulin resistance can be a chronic condition, it is possible to reverse!
According to the National Institutes of Health (NIH), "Taking small steps, such as eating healthier foods and moving more to lose weight can help reverse insulin resistance and prevent or delay type 2 diabetes in people with prediabetes."
Type 2 Diabetes & Insulin Resistance
Did you know that insulin resistance and type 2 diabetes are related? Here's how:
- Insulin is a hormone that is produced by the pancreas. Its main job is to control how your body uses and stores blood sugar (also known as glucose).
- Insulin resistance is a condition where the pancreas still produces adequate levels of insulin, but the cells don’t respond to it properly. More on this below.
- Type 2 diabetes is a consequence of chronic insulin resistance that hasn't been managed appropriately.
The good news? Type 2 diabetes can often be prevented (or have its onset delayed) by utilizing certain lifestyle strategies that help manage insulin resistance.
Are insulin resistance and prediabetes the same thing?
Insulin resistance and prediabetes are closely related conditions, but not the same. Many people are insulin resistant, but not all of them have diabetes. However, over time, insulin resistance often lead to prediabetes and, if not reversed, can turn into type 2 diabetes.
Did you know? In the United States, more than 84 million people ages 18 and older have prediabetes. That’s about 1 out of every 3 adults.
The Connection Between Diabetes & Fertility
Diabetes is not a foreign term when it comes to infertility, but not everyone knows why it happens, how it affects your body, and what you can do about it.
What does diabetes actually do to harm our fertility?
Researchers have found that women and men with elevated blood sugar and insulin resistance are at greater risk for fertility challenges. More specifically, poorly controlled hemoglobin A1c (blood sugar) levels are correlated with the following:
- Longer time to achieve a pregnancy
- Higher chance of pregnancy loss (miscarriage)
- Increased risk for birth defects in early pregnancy
How common is insulin resistance?
Insulin resistance is incredibly prevalent, with 40% of people in the U.S. battling the condition. It is not only the predecessor to type 2 diabetes - some researchers also believe that insulin resistance is at the root of many (if not most) chronic diseases.
But before we can fully understand insulin resistance, we need to explore what insulin is and the important role it plays in our bodies.
How Insulin Works
Insulin is a hormone that is produced by the pancreas. Its main job is to control how your body uses and stores blood sugar (glucose). It basically acts as the "key" that allows glucose to enter the cells where it is used for energy (see first image below).
During digestion, insulin stimulates muscle, fat, and liver cells to absorb that glucose. The cells either use the glucose for energy or, if there is too much glucose (as in the case of over-eating), store it as fat.
Understanding Insulin Resistance
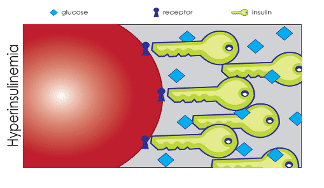
Insulin resistance is a condition where the pancreas produces adequate levels of insulin, but the cells don’t respond to it as they should. This results in the pancreas over-producing insulin, which is called compensatory hyperinsulinemia (see second image below) in an attempt to lower circulating blood glucose levels.
Over time, the pancreas tires of this excess secretion and doesn’t make enough insulin to keep blood glucose levels in the normal range. When this occurs, a person is officially diagnosed with diabetes.
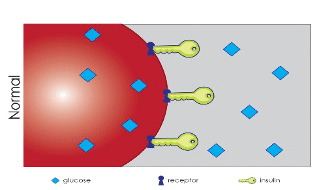
 Images courtesy of Fertile Health, LLC.
Images courtesy of Fertile Health, LLC.
How Insulin Resistance Affects the Body
Insulin resistance can have profound effects on the body. Let's discuss what they are:
Increases Production of Triglycerides
Insulin resistance causes fat cells to expand to accommodate excess fat storage.
Once they can't expand any further, they release fatty acids into the bloodstream. Those fatty acids then travel to other organs that are not equipped to handle these fats, such as the liver and skeletal muscle. The liver then becomes overwhelmed with fat deposits and increases the production of triglycerides.
Causes Chronic Inflammation
The over-expansion of fat cells causes chronic inflammation, which further promotes insulin resistance. In those with polycystic ovary syndrome (PCOS), insulin resistance prevents the conversion of male hormones (androgens) into estrogen in the ovary, which causes an excess of androgens and inadequate levels of estrogen to trigger ovulation.
This typically results in:
- Irregular menstrual cycles
- Androgenic symptoms (i.e. excess body hair, acne, hair loss)
- Inability to recognize satiety (when you are full)
Affects Ability to Sense Hunger/Fullness
Perhaps one of the most frustrating aspects of insulin resistance is the vicious cycle it sparks.
Once insulin resistance occurs, it can lead to overeating, which can lead to excess weight gain, which can lead to increased inflammation, which then promotes insulin resistance. And now we’re back at the beginning of the cycle.
How does insulin resistance cause weight gain?
In the presence of excess weight, insulin resistance can also lead to leptin resistance (leptin is a hormone that signals to the brain that you are full). When the brain is resistant to leptin, hunger and satiety signals are disrupted.
So, even though someone eats an adequate amount of food, the brain doesn't perceive this, leading to overeating, which can lead to excess weight, which leads to inflammation and worsening insulin resistance.
Excess weight (particularly in the abdominal area) can cause insulin resistance to worsen, so it is important to try to achieve a healthy weight. Losing just 5-7% of your starting weight can significantly reduce your chance of developing diabetes.
It feels like insulin resistance does everything in its power to continue this cycle. While this can be overwhelming and frustrating to learn, once you do, you can begin exploring the many different ways to combat it.
Ways to Treat Insulin Resistance
Put simply, the goal of treating insulin resistance is to make the cells more sensitive to insulin. There are some medications that can help with this, including Metformin and GLP-1 drugs like Mounjaro or Wegovy, but the primary way is through lifestyle changes.
Here are some helpful, research-based strategies to consider:
Minimize Glucose Spikes
Try to eat in a way that minimizes glucose (and insulin) spikes. Be conscious (though not restrictive) about limiting sugar and overly processed foods (such as chips, crackers, and cookies) since each time you ingest these, they cause a jump in glucose and, therefore, insulin.
When making a meal or snack, start with a healthy animal or plant-based protein, add fruit or vegetables, and a healthy fat (if not found in your protein source). For example, an apple with almond butter.
Tip: When choosing a carb, make sure it's as close to its natural form as possible. Think brown rice instead of white rice and whole wheat pasta instead of white pasta, etc.
Try the Mediterranean Diet
An adaptation of the Mediterranean diet, which encourages moderate intake of monosaturated fats (such as those found in extra virgin olive oil and avocado) is often recommended for those with insulin resistance.
The addition of Omega-3 fatty acids (found in oily fish, such as salmon, or an Omega-3 supplement) and avoiding trans fats (often found in processed foods) are also important, as saturated fat can hinder the ability of insulin to allow glucose to enter the cells.
Consider Eating Plant-Based
Some researchers maintain that a mostly plant-based diet is best for the prevention and/or reversal of diabetes, but this has been disputed and might be difficult for some to follow. It is clear, though, that ensuring you have a wide variety of ‘color’ every meal (fruits and vegetables) is an important nutritional component, particularly if you have insulin resistance.
Start (or Maintain) a Regular Movement Practice
Exercise is the greatest insulin-sensitizing agent, even in the absence of weight loss. Regular exercise activates skeletal muscle (which is the key site for removing glucose from the bloodstream), enhancing the uptake of glucose out of the circulation and into the cells, where it belongs.
Here are a few reminders:
- The type of movement you do is not important, as long as you like it enough to do it most days of the week.
- A regular movement practice should include both cardio and strength training.
- Set yourself up for success by creating a visual cue (like putting a yoga mat near your bed, packing a gym bag, or putting sneakers near the door).
Like any new habit, getting started is hard. Physical activity becomes more rewarding the more you do it. So, at first it may seem tough to exercise every day, but after a few regular sessions, your body and brain will start to crave it.
Get Adequate Sleep
By adequate, we mean uninterrupted, quality sleep.
Poor sleep contributes to inflammation, which forces cells to create substances that make them more resistant to insulin (exactly the opposite of what we are hoping to achieve).
Most people require 8-10 hours of quality sleep, but the amount that you need may vary.
Need some sleep hacks? Check out these tips to encourage quality rest.
Identify Stress Management Strategies
Chronic stress affects all body systems and kicks off a cascade of hormones (like adrenaline and cortisol) that are insulin antagonists, meaning they "work against" insulin. Because a fertility journey itself can generate stress, it is important to investigate what methods of stress release work best for you.
Using exercise as your main form of stress release is ideal, as the body produces the above hormones to prepare you for "fight or flight." Your body naturally wants to mobilize you when those stress hormones are released, making movement a natural solution.
Here are some other stress-relieving options:
Meditation & Mindfulness
If you are new to these practices, we suggest using an app that offers guided meditation exercises (i.e. Calm, 10% Happier, or Insight Timer).
Remember that this is a practice, so don't beat yourself up if you find it hard to clear your mind right away. When you get distracted, try to just go back to thinking about your breath. You can’t really practice these techniques incorrectly, as long as you are doing them.
Yoga
This gentle, stress-reducing form of exercise offers great benefits for those navigating insulin resistance or other hormonal challenges. You can even find free yoga classes online (Yoga With Adriene is a wonderful place to start!)
Therapy
There is significant evidence that counseling and mental health support during a fertility journey can lower levels of stress hormones and inflammatory markers. Illume has a referral network of vetted mental health professionals - just ask your Care Team for recommendations!
Relaxing Activities
When you struggle with insulin resistance, there is a constant temptation to overeat in response to stress (which can then cause excess weight gain and worsen insulin resistance).
There are many other ways to "nourish" your body in addition to eating:
- Hot tea (especially peppermint or cinnamon)
- Aromatherapy or scented candles
- Listening to music or a podcast
- Reading a great book
Note: If you find yourself in the kitchen when you’re not hungry, ask yourself "What am I really feeling right now?" If the answer isn't genuine hunger, leave the room for awhile and try one of the above suggestions instead.
Start a Gratitude Practice
One of the best ways to reduce anxiety is to practice a sense of thankfulness on a regular basis. You can do this by journaling or simply thinking about three things you are grateful for before going to sleep. Journaling has the added benefit of helping get any stressful thoughts out of your head and onto a piece of paper!
You Can Fight Insulin Resistance
What we hope you take away from this guide is that insulin resistance, though frustrating, is treatable and manageable.
Practicing stress reduction techniques, reaching out for support, and adopting a healthy lifestyle will help improve your metabolic profile (internal environment) and support weight loss, which can improve both your health and your future baby's health.
You've got this.
Monica Moore is a board-certified Advanced Practice Nurse Practitioner, nurse educator and health coach who has been caring for patients at Illume Fertility for over 20 years. She is also the founder and lead educator at Fertile Health, LLC. Monica is passionate about taking care of the whole patient, believing in the importance of integrating comprehensive care. She has a special interest in PCOS and combating weight bias with education and advocacy.

